The goals of the Artis lab are to understand the regulatory mechanisms that control immune cell homeostasis at the body’s barrier surfaces. Employing diverse models of microbial colonization, pathogen infection and chronic inflammation, research in the Artis lab is examining how mammalian host genetics and signals derived from commensal microbial communities influence innate and adaptive immune responses in the skin, lung and intestine.
Studies from a number of labs including the Artis lab, have highlighted that differential colonization of the body’s barrier surfaces by defined commensal bacterial communities can have a profound effect on the development and function of distinct T helper cell populations including Th1, Th2, Th17 and regulatory T cells (Tregs). Dysregulation in the balance of these helper T cell populations can profoundly alter susceptibility to a number of chronic inflammatory diseases including allergy, asthma, arthritis, multiple sclerosis, psoriasis and inflammatory bowel disease. Research in the Artis lab is focusing on how host factors including expression of cytokines and cytokine receptors can influence the balance of helper T cell responses and the development of chronic inflammation.
Recent studies in the Artis lab indicate that innate lymphoid cells, an emerging population of innate cells that express proinflammatory cytokines, may also contribute to the pathogenesis of multiple chronic inflammatory diseases. Innate lymphoid cells are derived from a common Id2-dependent precursor and appear to influence immunity, inflammation and tissue repair and homeostasis in health and disease. Ongoing studies are examining the influence of host- and environmental-derived signals on the development and functions of innate lymphoid cells. The findings of these studies offer the potential to identify new therapeutic targets to limit infection, chronic inflammation and autoimmune diseases.
In addition to host-derived factors, an emerging hypothesis is that alterations in the acquisition and/or composition of beneficial commensal bacteria can profoundly impact helper T cell and innate lymphoid cell responses resulting in susceptibility to multiple infectious and inflammatory diseases. Metagenomic sequencing approaches in patient populations have revealed dysbiosis (alterations of commensal bacterial communities) in patients suffering from multiple inflammatory diseases including arthritis, multiple sclerosis, psoriasis or inflammatory bowel disease. Studies in murine model systems support a causal relationship between alterations in commensal bacteria and chronic inflammation. Studies in the Artis lab are employing germ-free mice and selective antibiotic treatment, coupled with pyrosequencing of bacterial communities, to interrogate the mechanisms through which signals derived from commensal bacteria can influence expression of proinflammatory cytokines and pathogenesis of chronic inflammatory diseases at multiple barrier surfaces.
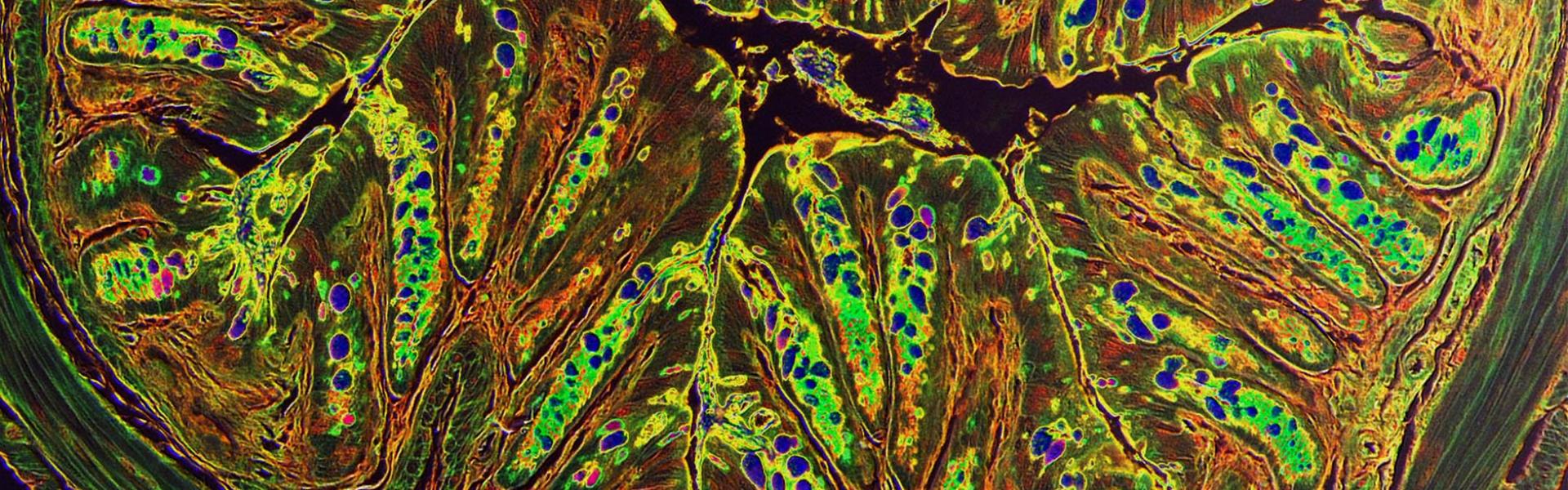
In a new series of studies, the Artis lab has forged a number of clinical collaborations and began to develop translational research approaches that will allow analysis of findings in murine model systems to be tested in patient populations. Employing tissue samples from clinically-defined patient populations, recent studies are examining the cellular sources of proinflammatory cytokines in the context of allergic diseases, inflammatory bowel disease or psoriasis. These approaches offer the potential to significantly advance our understanding of the pathogenesis of multiple chronic inflammatory diseases.